

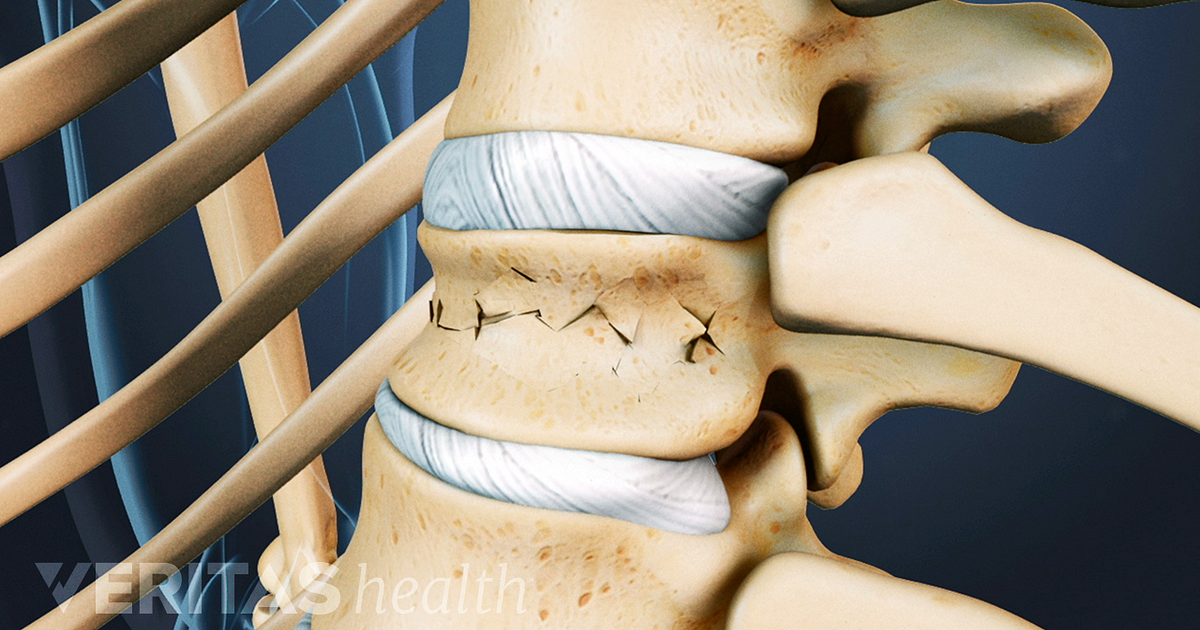
23 When symptomatic, patients complain of sudden-onset severe, focal, back pain that may radiate anteriorly and be confused with a cardiac or pulmonary process. Many fractures may develop insidiously and chronic compression fractures are commonly detected incidentally on chest X-rays. 16, 17 These patients are also at high risk of developing other significant osteoporotic fractures, such as hip fractures, 3 highlighting the need for early detection, treatment, and medical optimization of a patient’s bone quality and health. 1, 15įurthermore, the risk of developing a vertebral fracture is roughly five times greater if the patient has had a prior fracture, and 20% of osteoporotic postmenopausal women who present with an initial vertebral fracture develop a subsequent vertebral fracture within the year. 1, 14 It is estimated that more than a third of postmenopausal vertebral compression fractures occur in women who do not meet the criteria for osteoporosis. Though most commonly found among osteoporotic patients (T score ≤ −2.5 on dual-energy x-ray absorptiometry ), vertebral fractures may also occur in up to 18% of women > 60 years old with low bone mass but not meeting the criteria for osteoporosis (T score > −2.5 but <−1.4).
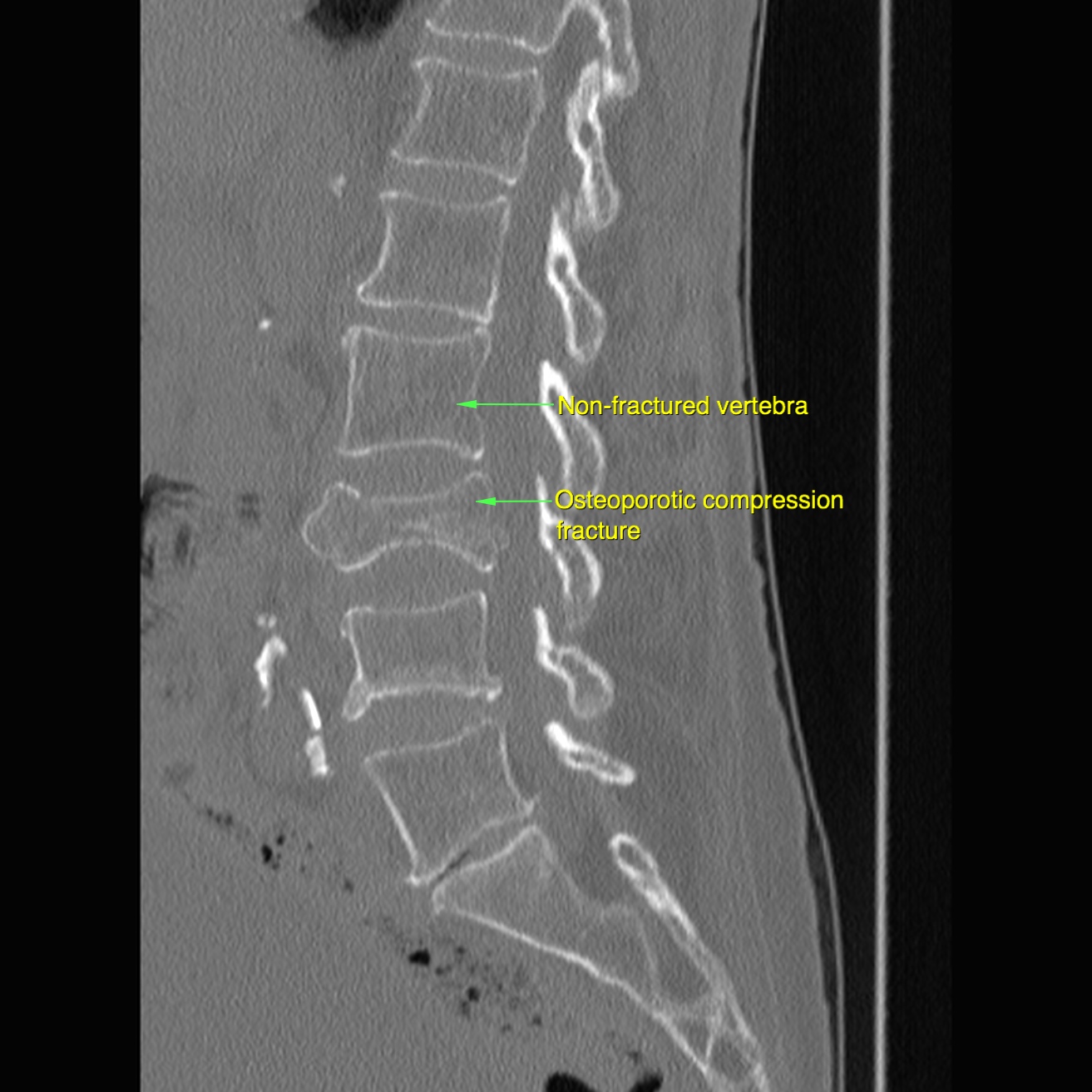
1, 3, 13 Occasionally, vertebral compression fractures may be the presenting finding for an underlying medical condition such as metastatic disease or hyperparathyroidism. These include lack of exercise and low body mass index, insufficient dietary calcium, low vitamin D production, glucocorticoid medication, smoking, and excessive alcohol intake. Though genetic predisposition and age of puberty onset play a significant role, a multitude of lifestyle and environmental factors increase the risk of developing osteoporosis. 1, 3 Bone density begins to decrease after age 40 for both men and women, and the process is rapidly accelerated in postmenopausal women. The risk of developing a vertebral fracture is strongly associated with decreasing bone density, with the risk increasing roughly two times for every standard deviation below average vertebral bone mineral density.
1, 10, 11 These age-correlated prevalence rates in the USA are very similar to those in Europe as published by the European Vertebral Osteoporosis Study. 7 – 9 The rate of vertebral fractures increases from an annual incidence of 0.9% and prevalence of 5%–10% among middle-aged women in their 50s to 60s, to an incidence of 1.7% and prevalence of greater than 30% among those 80 years and older. 1, 5, 6 Bone density of the vertebral column decreases steadily with age, with elderly women having lost almost half their axial bone mass by the time they reach their eighties. They most commonly occur among Caucasian women and are less common among men and women of African-American or Asian ethnicity. Vertebral fractures are directly correlated with increasing age and incidence of osteoporosis. 1 The actual incidence of vertebral fractures is likely much greater given the large number of vertebral fractures that go undetected, with only a third of vertebral fractures clinically diagnosed. Vertebral compression fractures are the most common sequelae of osteoporosis, comprising approximately 700,000 out of a total 1.5 million osteoporotic fractures annually in the USA.


 0 kommentar(er)
0 kommentar(er)
